Reproduction
Primary sex characteristics refer to changes to the sexual organs themselves (uterus, vagina, penis, and testes). Secondary sex characteristics refer to other visible changes that mark adult maturation such as changes in height and body shape. Primary sex characteristic changes for boys include the enlargement of the testes, penis, prostate gland, and seminal vesicles. These changes normally begin to occur between the ages of 9 and 14 years. Their growth is generally completed between ages 12 and 16 years.
The most significant and noticeable puberty-related change for young men is spermarche, or the first ejaculation. Spermarche generally occurs between the ages of 12 and 16. The spermarche indicates a boy is now producing sperm and could fertilize a female egg through sexual activity, resulting in female pregnancy. This first ejaculation often occurs during sleep; it is often referred to as a "wet dream." Young men may also experience spontaneous erections when they're awake. This may occur when they become emotionally stimulated, or for no reason at all. Such spontaneous erections can be uncomfortable or embarrassing for maturing young men.
The primary sex characteristic changes for girls includes the uterus starting to build a lining that will later be shed through the process of menstruation, and the vagina beginning to produce a mucus-like discharge. This mucus-like discharge is not actual menstruation but rather an early form of vaginal lubrication. As the young woman matures, she can produce this lubrication when she becomes sexually aroused, but she will also produce it in various quantities even when she's not sexually aroused. These changes can happen months or just weeks before a girl experiences menarche, or her first menstrual period. Every youth's experience is slightly different.
The most significant and noticeable primary sex change for young women is menarche, or the first menstrual period. This occurs when the uterus -- the organ that will later carry and nurture a baby -- sheds its first lining of tissue and blood. In adult women, this lining is shed once a month, or on average, every 28 days. The purpose of the lining is to condition the uterus for the initial portion of pregnancy in which a fertilized egg must attach to the uterine lining. The lining is shed each month when the body realizes it is not pregnant. Women are not "bleeding" when they have their menstrual period; there is no open wound. Instead, their uterus is simply shedding and releasing the bloody lining tissue that has grown inside it over the past month.
Menarche alone does not mean that a girl is able to become pregnant. In some cases pregnancy may occur prior to menarche, while in others it may not be possible for months after menarche. Some girls will not begin releasing eggs from their ovaries for up to 12 to 18 months after they begin their periods. Other girls will have begun releasing mature eggs prior to their first period. For this reason, young women need to be taught that it is possible (even if not common) for them to get pregnant before they have their first period if they should become sexually active.
On average, the first menstrual period occurs between ages 10 and 15 years for North American girls. While some girls may experience a full menstrual flow during their first period, some girls may only experience a light or spotty flow during their first periods. Young ladies may also experience very irregular period intervals and durations in the first months as their cycles regulate.
Download a pdf copy of Unit 10 - Human Reproduction and Development for offline use.
C$0.99
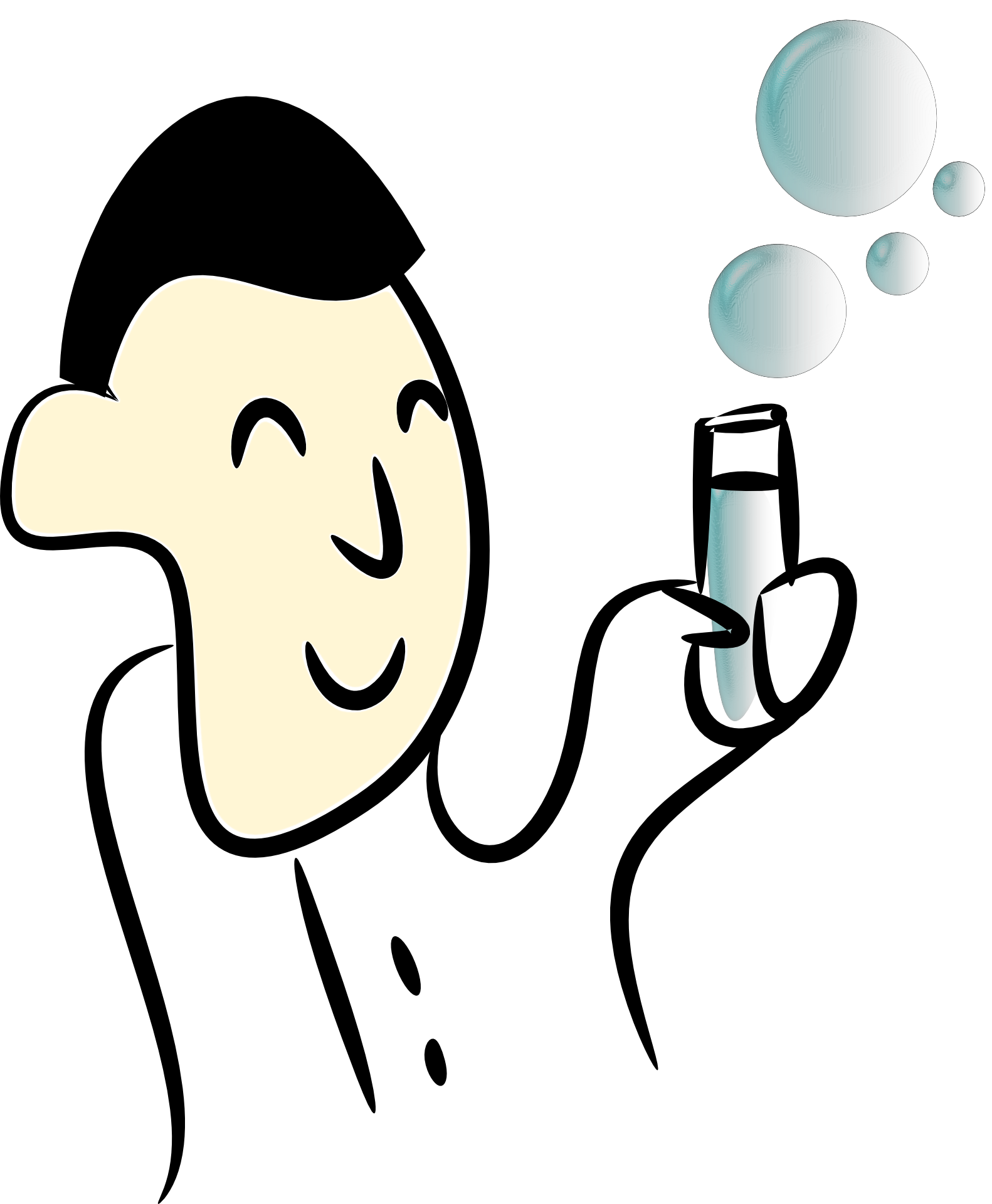
Testes: Male gonads that produce sperm. During the last two months of fetal development, the testes descend into the scrotum through a canal. A membrane forms over the canal so that the testes cannot re-enter the abdomen. The Scrotum is the sac that contains the testes. It helps to maintain the temperature a bit cooler than the abdominal cavity. This is important because sperms will not develop well/normally at body temperature.
The Vas deferens are the tubes that carry sperms from testes to the urethra. (Vasectomy is a surgical procedure that involves cutting the vas deferens. This prevents sperm produced in the testes to be in the ejaculated semen fluid. The semen fluid now only contains the secretions from the prostate and the seminal vesicles. This results in infertility. Tubal Ligation is done to females. The Fallopian tubes, which allow the sperm to fertilize the ovum and would carry the fertilized ovum to the uterus, are closed. This is sometimes referred to as getting one's 'tubes tied'. )
The Urethra is the channel for urine & semen. Semen (Seminal Fluid) is the fluid secreted by three glands and the sperm that travels along the vas deferens and the urethra.
Seminal Vesicle produces a fluids that contains fructose & prostaglandins. The fructose provides the sperm with a source of energy. The prostaglandins act as chemical messengers in the female system by triggering the rhythmic contraction of smooth muscle along the reproductive tract. This is thought to assist in the movement of sperm towards the egg/ova.
The Prostate Gland secretes an alkaline substance that protects sperm cells against the acidic environment of the vagina. The prostate fluid also nourishes the sperm. The Cowper's Gland (Bulbourethral gland) secretes an alkaline mucous The fluid excreted by these glands is clear and thick and acts as a lubricant; it is also thought to function as a flushing agent that washes out the urethra before the semen is ejaculated; it may also help to make the semen less watery and to provide a suitable living environment for the sperm.
The male reproductive System. (Source: Wikipedia, CC BY-SA 3.0)
In General, semen is - 60% secretions from the seminal vesicle, 30% secretions from the prostate gland and 10% secretions from the Cowper's gland.
The ejaculatory duct regulates the movement of semen into the urethra. The urethra also serves as a pathway for urine. A sphincter regulates the voiding of urine from the bladder. At any given time, the urethra conducts either semen or urine, but never both. Erection is achieved as a result of blood flow into erectile tissue of the penis. Stimulation of the parasympathetic nervous system causes the arteries leading to the penis to dilate, therefore increasing blood flow. Veins that carry blood away from the penis become compressed. Ejaculation of semen is caused by stimulation of the sympathetic nervous system.
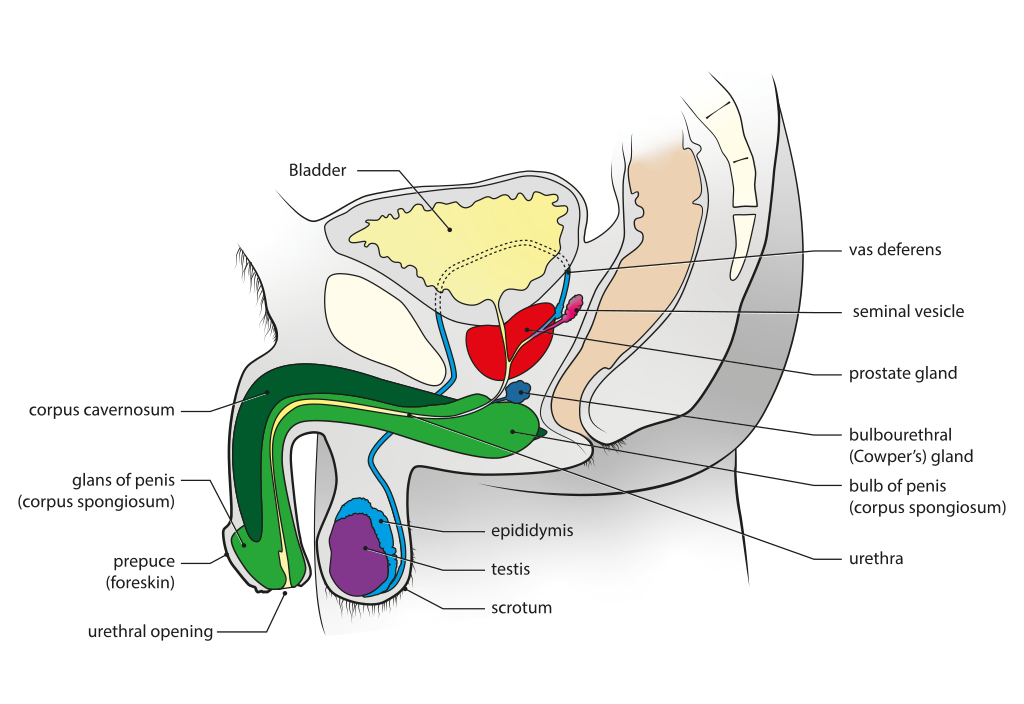
The Sperm Cell
Sperms are haploid, they contain 23 chromosomes in the nucleus (head). The Acrosome is a cap at the top of the head filled with a enzyme that is used to digest / dissolve the outer coating of the egg. The sperm has very minimal cytoplasm since it is streamlined. Stored sugars and numerous mitochondria are located in the midsection, to metabolize and supply energy needed for swimming up the female tract. The Flagellum (tail) is a long whip-like structure that helps in movement (swimming) of the sperm.
The structure of the sperm cell. (Source: https://socratic.org)
The production of sperms/spermatozoa is called Spermatogenesis. It occurs in the testes. The inside of each testis is filled with twisting tubules called seminiferous tubules. These tubules are lined with sperm producing cells called spermatogonia (spermatogenic stem cells), which are diploid, containing 46 chromosomes in humans. Spermatogonia divide via the process of meiosis to form spermatocytes, which are haploid, containing 23 chromosomes in humans.
The spermatogenesis process can be divided into five steps with the main cell types being:
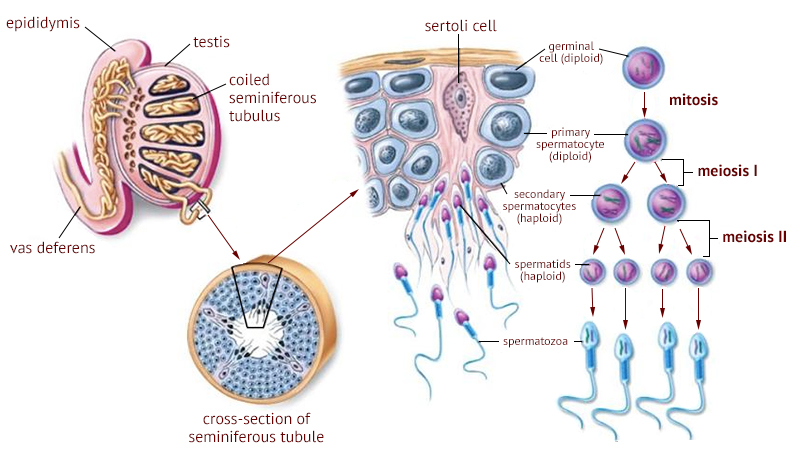
A detailed illustration of the spermatogenesis process and where it occurs. (Source: Philpot Education at https://www.philpoteducation.com/)
The main hormone involved in the development of the male reproductive system is Testosterone. Testosterone is produced in the interstitial cells of the testes. These cells are found between the seminiferous tubules. Testosterone has two main functions including stimulating spermatogenesis and influencing the development of secondary sex characteristics at puberty. Testosterone works in a negative feedback mechanism similar to other homeostatic hormones. High levels of testosterone increases sperm production. Once high levels of testosterone are detected, the hypothalamus mediates the negative feedback, which is executed by the pituitary gland.
Testosterones can also be used as anabolic steroids because they promote muscle build up.
The Sperm's Journey starts from the deposition of semen in the vagina. From there, they swim from the vagina > cervix > uterus > fallopian tube.
The female reproductive system is built to receive spermatozoa from the males, and create a conducive environment for the development of a fetus to term.
Ovaries are the female gonads. They produce hormones such as Estrogen and Progesterone and also serve as the site for oogenesis. Each ovary contains follicles, which are structures that contain the oocyte (egg) & granulosa cells. An Oogonium, containing 46 chromosomes, undergoes meiosis and is transformed into a mature oocyte or ovum (egg). Granulosa cells provide nutrients for the oocyte.
Fallopian tubes (oviducts) are the channels connecting the ovaries to the uterus. Fertilization occurs in the oviducts. An egg enters the tube from the ovary, via the fimbriae (finger-like structures at opening of the Fallopian tubes).
The Uterus is a hollow, inverted, pear shaped organ. It is the site where the embryo and fetus develop. The uterus is composed of three layers: Perimetrium, Myometrium and Endometrium. The Perimetrium is the outer layer composed of connective tissue. The Myometrium is the Muscular outer lining that provides support for the developing embryo. Contractions of this layer help to push the baby out. The Endometrium is the Glandular inner lining that produces endometrium every 28 days. If fertilization does not occur, the endometrium is shed (menstruation). The endometrium provides nourishment for the developing embryo.
The Cervix is a muscular band that separates the vagina from the uterus.
The Vagina connects uterus to outer environment. It is also called the Birth canal. It usually has a strongly acidic pH.
A female is born with all the egg cells that she will ever have. They are immature primary oocytes and only develop into mature egg cells when the woman enters sexual maturity.
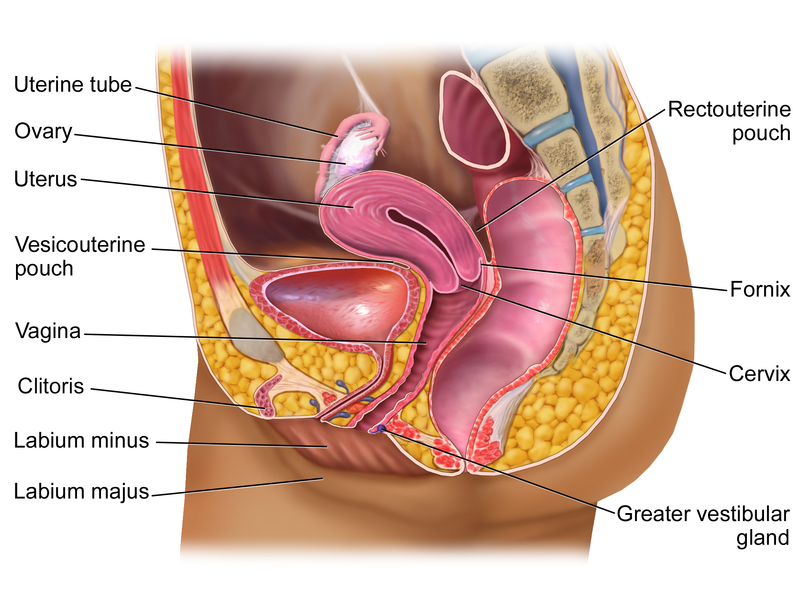
The female reproductive system. (Source: Wikipedia, CC BY-SA 4.0)
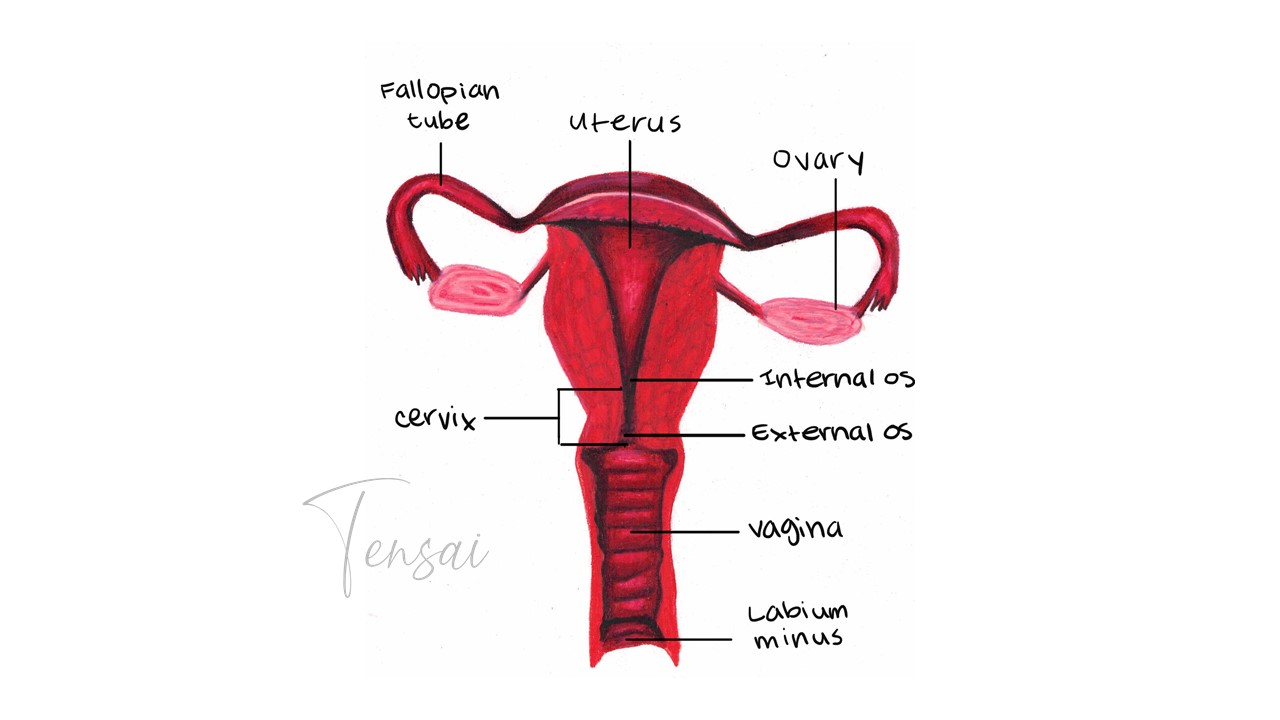
The female reproductive system.
Oogenesis refers to the differentiation of the ovum/ egg cell in females. Oogenesis starts with a germ cell, called an oogonium (plural: oogonia). The process begins in female embryos before they are born. At birth, all embryos already have all the primary oocytes they will need during their lifetime, which is about one to two million cells / primary oocytes.
At the onset of puberty, meiosis continues with the formation of a secondary oocyte and the release of one polar body. The Secondary Oocyte is the arrested at Metaphase II. At ovulation, this secondary oocyte will be released and travel toward the uterus through the oviduct. If fertilization occurs, Meiosis II is completed and the second polar body is released.
Polar bodies are small cells lacking cytoplasm. This is because the oocyte takes the larger portion of the cytoplasm (organelles) to enable it to sustain itself if fertilization occurs. Polar bodies are a way to get rid of the DNA without taking away the rest of the organelles.
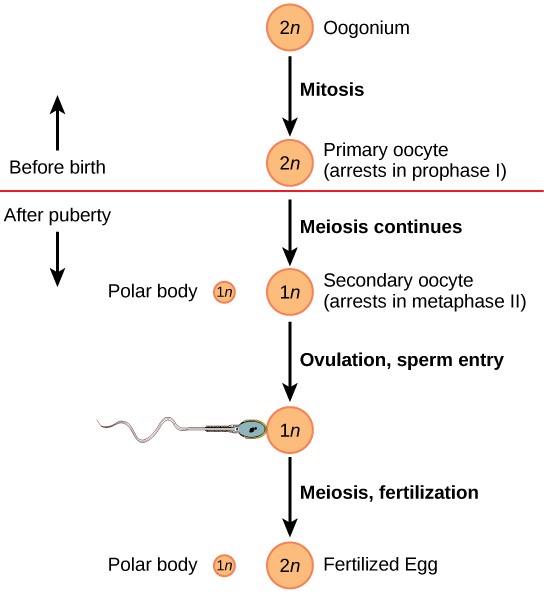
A brief illustration of the Oogenesis process. (Source: https://bio.libretexts.org/)
The female menstrual cycle takes an average of 28 days with some variation being common. The cycle occurs in four phases if no fertilization occurs:
The onset of female puberty causes the release of GnRH (Gonadotropin Releasing Hormone) from the hypothalamus. GnRH stimulates the anterior pituitary to release Follicle Stimulating Hormone (FSH) and Luteinizing Hormone (LH), which are then directed to the ovaries. During the follicular phase of the menstrual cycle, FSH secretions are carried by the blood to the ovary, where follicle development is stimulated. The developing oocyte begin to secrete estrogen. Estrogen is the major sex hormone in females. Its responsible for the development of breasts & body hair and increased thickening of endometrium. Estrogen also has an effect on metabolism, favoring more fat storage than muscle. It's also responsible for the thickening of vaginal wall, vaginal lubrication, maintenance of vessels and skin texture, reduces bowel movement. Estrogen promotes sexual receptivity during ovulation (estrus/heat in animals) and regulates the sexual receptivity behavior including lordosis in animals. Estrogens are also necessary for sex drive in males working in sync with Testosterone.
The production of estrogen and progesterone (hormones of the ovary) is regulated by the hypothalamus-pituitary complex. Gonadotropins (female FSH and LH) regulate the control of hormones produced by the ovary. As estrogen levels rise, a negative feedback mechanism is triggered, which induces the pituitary to turn off FSH secretions. On the other hand, estrogen causes a positive feedback mechanism on the secretion of LH, which is released when estrogen levels are high. Ovulation occurs at the end of the follicular phase when LH levels are highest.
The Luteinizing hormone causes the corpus luteum to secrete estrogen and progesterone. As progesterone and estrogen build up, another negative feedback mechanism is activated which inhibits the release of FSH, LH and GnRH.
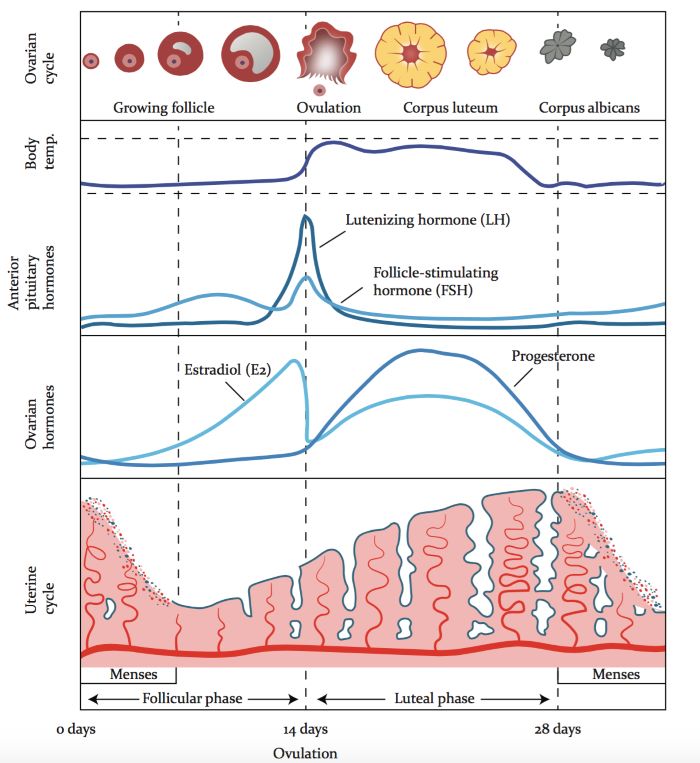
A detailed illustration of the menstrual cycle in females including the hormonal regulation of each stage of the cycle. (Source: Vios Fertility Institute, https://viosfertility.com/)
One ejaculate contains about 150-300 million sperm cells which can live 3-5 days in the female body. Only about 100 sperms will make it close to an egg. The egg (oocyte) is surrounded by 2 layers called the corona radiata and the zona pellucida, both of which must be penetrated by sperm before the egg is fertilized. There are receptors on the oocyte membrane that participate in the binding of the sperm and the egg.
To penetrate the egg, the sperm has an enzyme enclosed in the acrosome. Firstly, the sperm binds to the wall of the ova, and the acrosome membrane opens releasing the acrosome granules, these granules digest the egg wall allowing the sperm nucleus to penetrate/enter the ovum. Once the sperm has entered, the cortical reaction occurs. A surge in intracellular calcium activates the oocyte to prepare for cell division. It also causes the cortical granules, located just under the plasma membrane, to spill their contents into the extra cellular space beneath the zona pellucida. The spilled material binds water, and as it swells, it detaches all sperm still in contact with the oocyte membrane, accomplishing the permanent slow block to polyspermy. In rare cases of polyspermy that do occur, the embryos contain too much genetic material and are nonviable. The fertilized egg is now called the zygote and is diploid.
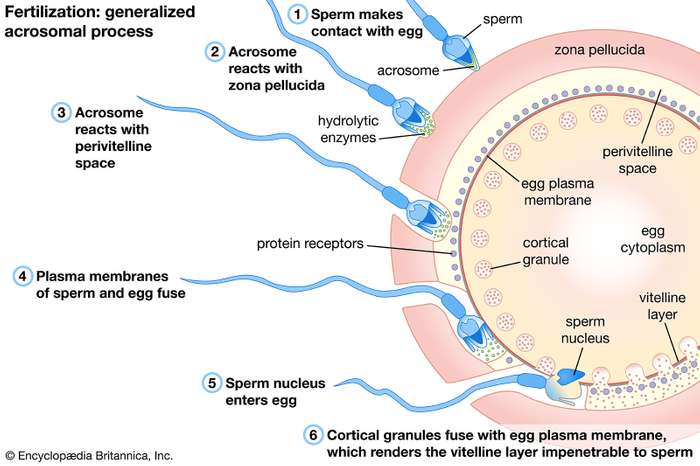
Fertilization: Steps associated with the entry of the sperm into the egg. (Source: https://www.britannica.com/)
The zygote moves down the fallopian tube (oviduct), towards the uterus, with mitosis occurring along the way. After a few days, a morula is formed from the zygote. A morula is a solid ball of cells (blastomeres) produced by cleavage. Cleavage occurs as Mitotic divisions but no cell growth so cells get smaller with each successive division.
At day 5, 6, or 7 after fertilization (conception), the embryo is called a blastocyst, 'a hollow ball of cells'; the blastocyst consists of a ring of outer cells called the trophoblast (supporting cells) and a clump of cells at one end inside the inner cell mass, which will become the embryo.
A blastocyct contains a disk of cells at one end, which will form the baby. The outer layer of cells will form the chorion, which will form the placenta, the exchange site between baby and mom. The cavity enclosed by the outer cell layer is the blastocoel.
For pregnancy to continue, progesterone and estrogen levels must be maintained, and not drop, otherwise, uterine contractions will occur and the embryo will be lost.
The chorion (outer cells layer) of blastocyst will develop finger-like structures called villi that grow into the endometrium. This process is called Implantation. The chorion secretes HCG (human chorionic gonadotropin) which stimulates the corpus luteum to maintain the endometrium (through estrogen and progesterone). The CL remains for about 3 months until the placenta is formed. Pregnancy tests detect levels of HCG.
The blastocyst (trophoblast) implants in the endometrium of the uterus about 6 or 7 days after fertilization.
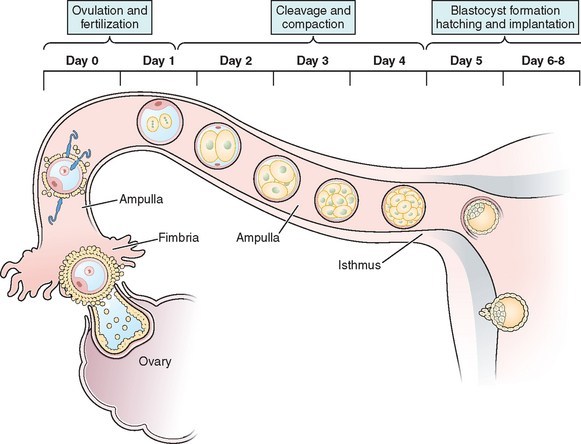
Fertilization and Implantation in humans. (Source: https://abdominalkey.com/)
Fraternal twins would form if two eggs were released during ovulation, and were both fertilized by two separate sperm cells.
Zygotes that twin at the earliest stages will be diamniotic and dichorionic. Twinning between 4 to 8 days after fertilization typically results in monochorionic-diamniotic twins. Twinning between 8 to 12 days after fertilization will usually result in monochorionic-monoamniotic twins. Twinning after 12 days post-fertilization will typically result in conjoined twins.
Monozygotic twins are genetically identical unless there has been a mutation in development, and they are usually the same gender. (On extremely rare occasions, an original XXY zygote may form monozygotic boy/girl twins by dropping the Y chromosome for one twin and the extra X chromosome for the other.) Examination of details such as fingerprints can tell them apart. As they mature, identical twins often become less alike because of lifestyle choices or external influences.
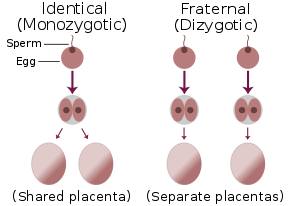
Identical versus Fraternal twins. (Source: Wikipedia, CC BY-SA 3.0)
There are nine months of pregnancy (~40 weeks from the date of the mother's last menstrual period, or ~38 weeks from conception) and it is broken down into THREE trimesters.
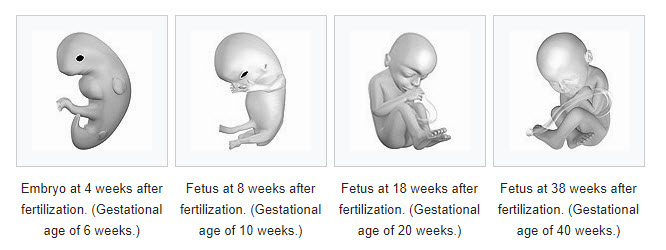
Fetal development. (Source: Wikipedia, https://en.wikipedia.org/wiki/Pregnancy)
The uterine contractions are caused by a drop in progesterone level and this has a positive feedback effect on the secretion of oxytocin (by the posterior pituitary), signaling the beginning of labor. oxytocin release is a positive feedback cycle; emotional and physical stress due to uterine contractions cause the release of more oxytocin. It is thought that there may be a chemical released by the fetus (a lung protein, signaling that the baby is developed enough to breathe outside the uterus) that causes a drop in progesterone.
False labor (Braxton Hicks contractions) can occur through the third trimester and near the beginning of labor when progesterone levels are initially dropping. the hormone relaxin, produced by the placenta, is secreted prior to labor to help loosen the pelvic ligaments. The mother's cervix becomes thin and begins to dilate as the baby's head pushes on it. The amniotic membrane bursts and amniotic fluid lubricates the canal, the so called 'Water breaking'. As the baby progresses through the birth canal, contractions become stronger and more frequent, until the baby is born. Labor can last from 2-24+ hours. Once the baby is born, the umbilical cord is clamped and cut.
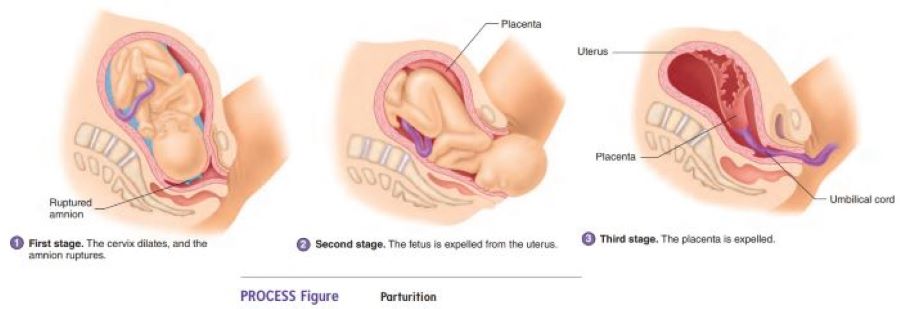
Stages in the process of giving birth. (Source: https://www.brainkart.com/)
After the baby is born, the placenta detaches from the uterus wall and is expelled from the birth canal (after birth). It is important that the entire placenta detaches and gets expelled because open wounds in the uterus may result in excessive bleeding and sometimes leads to death. The placenta is checked by a doctor to ensure that the entire placenta has detached.
During pregnancy, estrogen and progesterone levels help prepare the breast for milk production. Each breast contains around 20 lobes of glandular tissue, each with a duct which carries milk to the nipple. Expulsion of the placenta causes the hormone prolactin to be released by the anterior pituitary. Prolactin stimulates the glands within the breast to produce milk. Prolactin increases during pregnancy but milk production is suppressed by high levels of estrogen & progesterone from the placenta because these hormones inhibit Prolactin.
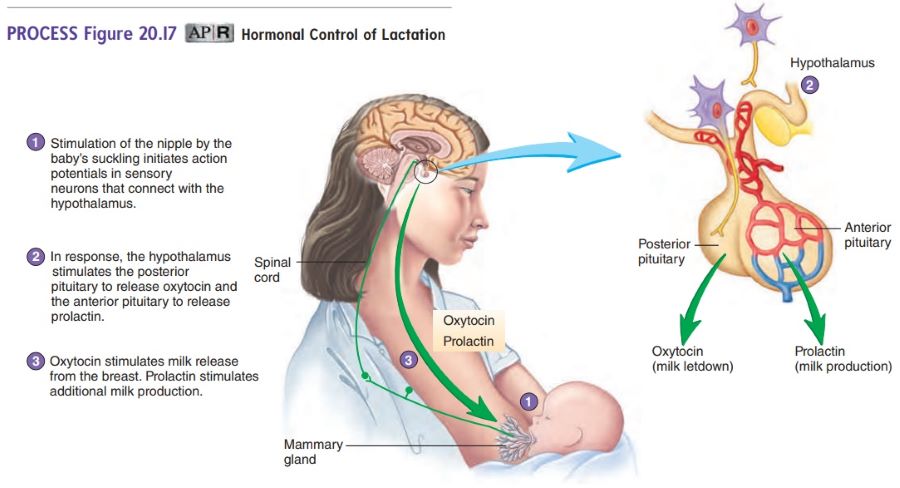
Hormones and feeback mechanisms involved in lactation. (Source: https://www.brainkart.com/)
The first milk is a few drops of clear fluid called colostrum. This is rich in antibodies to give temporary immunity. When prolactin levels increase after the birth of a child, this stimulates the addition of milk fat to the breast milk. Breast milk does not flow easily. The suckling action of a newborn stimulates the nerves endings in the areola (dark part) of the breast. This causes the release of oxytocin from the posterior pituitary. Oxytocin causes weak contractions of the glands in the breast (myoepithelial cells), helping the milk move towards the nipple. The oxytocin that is released by the baby breastfeeding also helps the uterus of a mother to return to its original shape and size because it causes the uterus to contract slightly.
On average, mothers can produce up to 1.5L of milk per day. The mother must ensure that her diet contains many nutrients, especially calcium, since 2-3g of calcium and phosphate are released through breast milk. Breast milk also contains antibodies to help a child develop immunity.
IVF involves removing eggs from the ovaries (donor) fertilizing them in the laboratory (in vitro) and then planting the embryos into the uterus of a surrogate mother/recipient, where they implant and mature. Various hormone medications are administered in the treatment cycle to enhance the growth and maturation of the follicles, thereby improving chances for fertilization and control the timing of ovulation so eggs can be retrieved before they are spontaneously released. Multiple pregnancies are the most common complication occurring in about 20% of IVF cases, since more that one embryo is usually implanted.
Are used to stimulate follicle production in men and/or women. It increases the number of eggs or sperm produced. Often used prior to IVF to stimulate egg development.
A small amount of amniotic fluid is drawn from the mother’s uterus (using a long needle, going through the woman’s belly). This fluid is genetically tested for disorders (usually chromosomal). Can be preformed in weeks 15-18 of pregnancy. There is a chance of miscarriage with this procedure.
Similar to amniocentesis but the needle draws out placental cells rather than amniotic fluid. This test can be performed as early as 10 weeks, but also carries the risk of miscarriage. Unlike amniocentesis, CVS is unable to test for neural tube defects.
The technique uses sound waves to study and treat hard-to-reach body areas. In scanning with ultrasound, high-frequency sound waves are transmitted to the area of interest and the returning echoes recorded by a sonograph, which produces an image.
Occurs when live sperm are inserted into an ovulating female for the purpose of initiating fertilization.
Stem cells are primitive cells that give rise to other types of cells. These cells are undifferentiated and contain all of the genetic information needed to create any cell type in the body. Because of their undifferentiated state, they are less prone to rejection because they lack the features that would allow them to be recognized by the recipient’s immune system. Stem cells can be used to help treat diseases such as leukemia, lymphoma and anemia.
The test is done in pregnant females. Low levels of this protein may indicate Down Syndrome. High levels may indicate neural tube disorders i.e. Spina bifida.
The Rhesus protein is part of the blood type proteins. A person can be rhesus positive, if they have the protein, or Rhesus Negative, if they lack the protein. When a RH negative women carries a RH positive baby, it means the two are incompatible. During the labor process, if the babies blood mixes with the mother's blood an immune reaction will ne initiated so that the mother will now have Anti-RH+ antibodies. If the mum gets pregnant again with a RH+ baby, her blood will cross the placenta and attack/harm the fetal blood cells causing anemia and possibly death. RH -ve women are now given anti-RH serum (RHoGAM) after first birth to destroy antigens and prevent formation of antibodies.
Occurs when the developing zygote implants in the fallopian tubes, rather than the endometrium. The embryo develops there and this causes great risk to both the mother and the baby, and usually cannot be rescued.
Types of ectopic pregnancies.
Download a pdf copy of Unit 10 - Human Reproduction and Development for offline use.
C$0.99
At the time of delivery the fetal buttocks are the presenting part in the maternal pelvis. Frank breech is when the fetal hips are flexed and the knees extended with the feet near the shoulders, accounting for 60-65% of breech presentations at term. Incomplete breech occurs when one or both of the fetal hips are incompletely flexed, resulting in some part of the fetal lower extremity as the presenting part. Thus the terms single footling, double footling, knee presentation. Accounts for 25-35% of breech presentations. Complete breech is similar to frank breech except one or both knees are flexed rather than extended. Accounts for 5% of breech presentations. The doctor may attempt to shift its position by applying pressure to the abdominal wall and manipulating the fetus in an attempt to turn it. This process is called an external cephalic version (ECV). In some cases, babies are delivered breech. Recent studies have shown that heat acupuncture treatments can be used on the woman's feet in order to stimulate the baby to turn into the right position for delivery. In cases where delivery cannot be preformed, and the baby does not turn over, a caesarian section is performed.
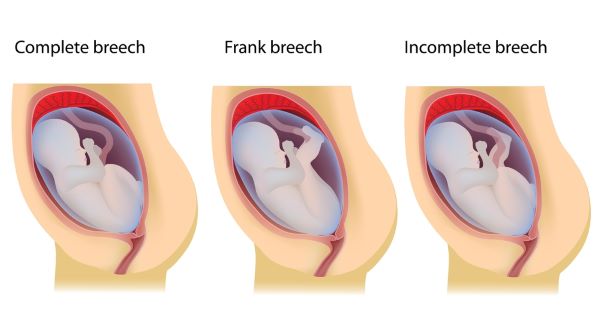
Types of breech presentations. (Source: https://americanpregnancy.org/)
When placenta lies low in the uterus. Painless vaginal bleeding is a sign. Diagnosed by ultrasound. Baby should not be delivered vaginally if the placenta previa persists at term.
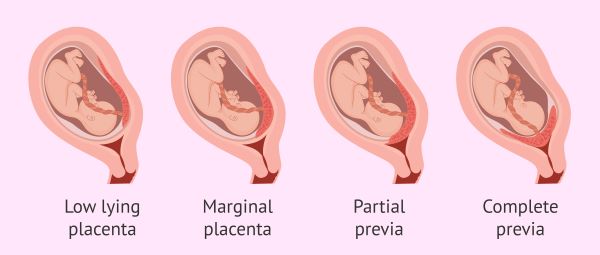
Varying degrees of Placenta Previa. (Source: https://www.invitra.com/)
In this procedure, a doctor makes an incision in a woman's abdomen and uterus and removes her baby through it.
You can access Tensai High School Biology revision questions HERE